Aptima® HPV Assay and Aptima® HPV 16 18/45 Genotype Assay
The only FDA approved mRNA-based HPV Assays.
Overview
Documents
Training
Don't Just Sense Presence, Sense a Threat
The Aptima® HPV Assay and Aptima® HPV 16 18/45 Genotype Assay are molecular tests used in the detection of the human papillomavirus present in cervical samples. Powered by mRNA-based technology, they help detect both the presence and activity of high-risk HPV infections – offering equivalent sensitivity to DNA-based tests, with increased specificity.1-16
Increased Specificity
Multiple studies have demonstrated that the Aptima HPV Assay provides equivalent sensitivity to DNA-based tests, with increased specificity.1-16
Fewer False Positives
By targeting E6/E7 oncoproteins, the assays can identify the infections most likely to lead to disease — resulting in 24%-40% fewer false positives compared to DNA-based tests.17-19
Decade of Data
The Aptima mRNA-based HPV assays showed extensive longitudinal safety data up to 10 years.11, 12, 20-22
Benefits of mRNA Testing
mRNA based-technology helps to identify the infections most likely to lead to cervical cancer – supporting informed decision making and enabling laboratories and healthcare professionals to receive accurate and actionable results.17,18
A targeted and evidence-driven approach to molecular HPV testing.
Targeted 16 18/45 genotyping, backed by data, identifies the infections associated with the highest risk of disease.17,18
Up to 80% of squamous cell carcinomas are associated with HPV 16, 18, 45.23
Up to 92% of HPV-related adenocarcinomas are associated with HPV 16, 18, 45.23
Aptima HPV Assay
Identifies active high-risk HPV Infections
Test for all 14 high-risk genotypes with a single specimen. mRNA technology maximizes screening benefits while minimizing false positives for confidence in your results.1
Aptima HPV 16 18,45 Genotype Assay
Targets the critical HPV genotypes
Detect HPV genotypes 16, and 18 or 45, which are associated with most squamous cell carcinomas and HPV-related adenocarcinomas. Run both assays from the same specimen tube for greater flexibility.24
The Aptima HPV Assay is FDA approved to support multiple screening modalities, providing flexibility in testing options.
Co-testing
Primary screening
Reflex testing of ASC-US cytology results
With the Aptima HPV Assays, laboratories employ a validated, standardized and flexible workflow for HPV testing.
Explore our Total Cervical Health portfolio to learn more about Hologic’s comprehensive offering for cervical cancer screening.
1. Aptima HPV Assay. US package insert AW-33883-001. Hologic, Inc.; 2026. 2. Saslow D, et al. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology Screening Guidelines for the Prevention and Early Detection of Cervical Cancer.Am J Clin Pathol 2012;137:516-542. 3. Wu R, et al. Human papillomavirus messenger RNA assay for cervical cancer screening: the Shenzhen Cervical Cancer Screening Trial I. Int J Gynecol Cancer. 2010;20(8):1411-1414. 4. Ratnum S, et al. Aptima HPV E6/E7 mRNA test is as sensitive as hc2 Assay but more specific at detecting cervical precancer and cancer. J Clin Microbiol. 2011;49(2):557-564. 5. Monsonego J, et al. Evaluation of oncogenic human papillomavirus RNA and DNA tests with liquid-based cytology in primary cervical cancer screening: the FASE study. Int J Cancer. 2011,129(3):691-701. 6. Iftner T, et al. GAST: German Aptima Screening Trial. Comparison of Aptima and hc2 in routine screening in Germany. Symposium presentation at EUROGIN 2012. 7. Cuzick J, et al. Comparing the performance of six human papillomavirus tests in a screening population. British J Cancer. 2013;108:908-913. 8. Nieves L, et al. Primary Cervical Cancer Screening and Triage Using an mRNA Human Papillomavirus Assay and Visual Inspection. Int J Gynecol Cancer. 2013;23:513-518. 9. Iftner T, et al. Head-to-Head Comparison of the RNA-Based Aptima Human Papillomavirus (HPV) Assay and the DNABased Hybrid Capture 2 HPV Test in a Routine Screening Population of Women Aged 30 to 60 Years in Germany. J Clin Microbiol. 2015;53(8):2509-2516. 10. Muangto T, et al. Experience of combined liquid based cervical cytology and high-risk HPV mRNA for cervical cancer screening in Thammasat University Hospital. Asian Pac J Cancer Prev. 2016;17(9):4409-4413. 11. Reid et al. Human Papillomavirus Oncogenic mRNA Testing for Cervical Cancer Screening. Am J Clin Pathol, 2015;144:473-483. 12. Cook et al., Aptima HPV Assay versus Hybrid Capture® 2 HPV test for primary cervical cancer screening in the HPV FOCAL trial J. Clin. Virol. 2017;87:23–29. 13. Cook et al. Cobas 4800 HPV and Hybrid Capture 2 comparison at baseline and 48 months in the HPV Focal trial. Poster presented at IPV 2017. 14. Rebolj et al. A daunting challenge: Human Papillomavirus assays and cytology in primary cervical screening of women below age 30 years. EU J of Cancer (2015) 51, 1456-1466. 15. White C, et al. Performance of the HPV E6/E7 mRNA Aptima HPV assay combined with partial genotyping compared with the HPV DNA Cobas 4800 HPV test for use in primary screening: Results from the CERVIVA HPV primary screening study in Ireland [published online ahead of print, 2023 Aug 26]. Int J Cancer. 2023;10.1002/ijc.34685. doi:10.1002/ ijc.34685. 16. Pi R, Li T, Zhang H, Zhou H, Yang Y, Dai Y, Wu Z, Jiang M, Chen W, Zhu L. The Distribution of HR-HPV E6/E7 DNA and mRNA by Histological Grade and the Clinical Performance for Detection of Cervical Cancer and Precancer. J Med Virol. 2024 Nov;96(11):e70026. doi: 10.1002/jmv.70026. PMID: 39540331. 17. Cuschieri, et al. Human papillomavirus type specific DNA and RNA persistence—implications for cervical disease progression and monitoring. J Med Virol. 2004;73:65-70. 18. Tinelli, et al. HPV viral activity by mRNA-HPV molecular analysis to screen the transforming infections in precancer cervical. 19. Doorbar J. Molecular biology of human papillomavirus infection and cervical cancer. Clin Sci (Lond). 2006 May;110(5):525-41. doi: 10.1042/ CS20050369. PMID: 16597322. 20. Cook et al., Comparative performance of human papillomavirus messenger RNA versus DNA screening tests at baseline and 48 months in the HPV FOCAL trial. J. Clin. Virol., 2018;108:32-37. https:// doi.org/10.1016/j.jcv.2018.09.004 21. Forslund O, et al. HPV mRNA and HPV-DNA detection in samples taken up to seven years before dysplasia of cervix uteri. Int J Cancer. 2018; doi: 10.1002/ijc.31819. 22. Strang T, et al. Long-term cervical precancer outcomes after a negative DNA-or RNA-based human papillomavirus test result. Am J ObstetGynecol. 2021 Nov;225(5):511.e1-511.e7. doi: 10.1016/j.ajog.2021.05.038. 23. Wei F, Georges D, Man I, Baussano I, Clifford GM. Causal attribution of human papillomavirus genotypes to invasive cervical cancer worldwide: a systematic analysis of the global literature. Lancet. 2024 Aug 3;404(10451):435-444. doi: 10.1016/S0140-6736(24)01097-3. PMID: 39097395. 24. Aptima HPV 16 18/45 Genotype Assay. US package insert AW-34502-001. Hologic, Inc.; 2026.
Safety Data Sheets
Package Inserts
Related Products

Overview
Package Inserts
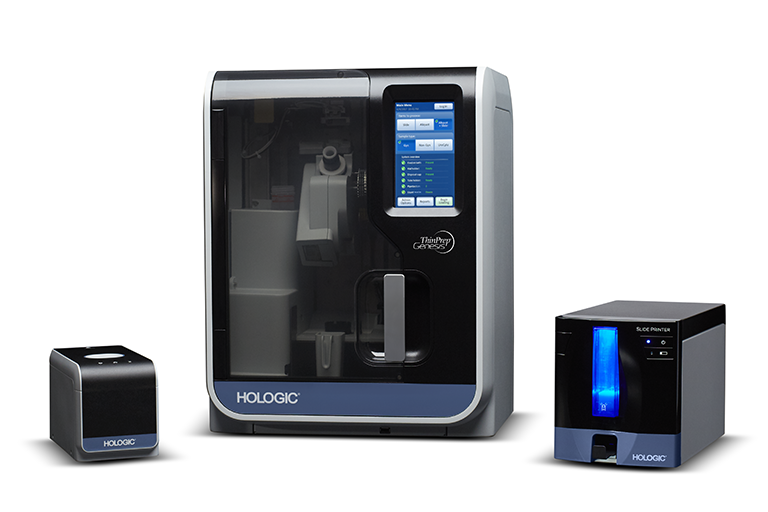
Leading the charge in cervical disease prevention with the ThinPrep system and Aptima HPV assays
Hologic has remained an unwavering advocate for women’s health for more than two decades. Our goals as a company are intrinsically tied to changes in best-practices for women’s health, applying the latest findings in diagnostic medicine to the development of new products and technologies in response to the emergence of new discoveries in medicine.
Cervical disease screening is an essential component of our efforts in women’s health. Hologic is the leader in Pap and human papillomavirus (HPV) testing. The ThinPrep Pap test helps healthcare providers detect the presence of abnormal cervical cells, and the Aptima HPV assays identify high-risk HPV mRNA that is indicative of the HPV infections most likely to lead to cervical disease.1-3
Today, screening with Pap+HPV Together (co-testing) provides the best possible protection against cervical cancer for women ages 30-65.4-6 Now, what was once a top cancer among women is up to 93% preventable.7
The introduction of the Pap smear and, later the ThinPrep Pap test, have contributed to a decline in cervical cancer rates of more than 60% since the 1950s.1,8 Since then, HPV has been identified as a cause of cervical cancer, and HPV testing and vaccinations have been developed.9
These medical triumphs have fortified the medical community’s ability to detect and prevent cervical disease and cancer. Today, the combination of data-supported guidelines for cervical cancer screening and the availability of HPV vaccination are key in the fight for women’s health.
Hologic released the first liquid-based cytology option in cervical disease screening in 1996: the ThinPrep Pap test.1 Today, more than 20 years after the release of the ThinPrep Pap test, it remains the preferred choice in Pap testing in the United States.10 ThinPrep Pap tests account for more than 80% of Pap tests performed in the United States, with 650 million tests performed globally so far.10
More than 170 scientific studies involving the ThinPrep Pap test have demonstrated its benefits, including increased disease detection, reduction of equivocal diagnoses, improved specimen adequacy, adjunctive molecular testing and morphology assessment.11
The College of American Pathologists reported increased HSIL (high-grade squamous intraepithelial lesions) and LSIL (low-grade squamous intraepithelial lesions) in labs using LBC versus labs that utilized conventional Pap testing.12 It also showed increased sensitivity for cervical adenocarcinoma over conventional Pap testing.13
The Aptima HPV assay and Aptima HPV 16 18/45 genotype assay target HPV types that pose the largest threat to women.2,3 While other HPV assays target DNA, the Aptima HPV assays target mRNA, which studies show reflects the presence and activity of high-risk HPV infection.2,3 The Aptima HPV assay detects E6/E7 mRNA, which is indicative of those HPV infections more likely to cause cervical disease.2 The Aptima HPV 16 18/45 genotype assay identifies HPV types 16, 18 and 45, which are associated with up to 80% of all invasive cervical cancers worldwide.3,14-15
Screening women with Aptima HPV assays helps providers optimize care for each patient.
The ThinPrep Pap test is just one of several offerings in the ThinPrep system. The ThinPrep processors, imagers and review scopes help improve workflow in laboratories and assist with cytotechnologists’ ability to identify abnormalities. These instruments help complete the ThinPrep system and maximize laboratory efficiency and accuracy in disease detection.
In addition to the ThinPrep Pap test, Hologic remains committed to providing laboratories with innovative and effective cytology solutions for non-gynecological testing needs.
Processors
Imagers and Review Scopes
Combines the power of ThinPrep imaging and manual microscope review in a single desktop system, with slides imaged and ready for review in approximately 90 seconds.
Identifies 22 areas of interest within the ThinPrep Pap test slides with the largest, darkest nuclei for cytotechnologists to examine.
Same trusted algorithm as the ThinPrep image processor, but with a faster camera, expanded label-reading formats and on-demand imaging.
Presents the 22 fields of view to the cytotechnologist for their review.
Combines the power of the review scope with the flexibility of a manual microscope.
Stainers
Now Available Compass Stainer: Adds flexibility to both routine and special staining procedures. Comes programmed with the ThinPrep Stain Protocol for customer convenience.
From Pap and HPV testing to our full range of diagnostic products and cross-divisional innovations like the Genius™ 3D Mammography exam for breast health, Hologic delivers for women. Our promise to offer innovative products to meet the needs of women globally persists throughout all that we do, including in cervical disease screening. Working together, we can achieve the goal of defeating cervical disease.